AMERICAN HEART ASSOCIATION UPDATES:
Please note that periodically AHA updates its Emergency Cardiac Care (ECC) guidelines which are immeidately included in this course to ensure that the information you receive is fully up-to-date and that your certification is in full compliance. If you wish to read these updates, [click here].
Please note that periodically AHA updates its Emergency Cardiac Care (ECC) guidelines which are immeidately included in this course to ensure that the information you receive is fully up-to-date and that your certification is in full compliance. If you wish to read these updates, [click here].
INTRODUCTION
Statistics indicate that sudden cardiac arrest (SCA) is rapidly becoming the leading cause of death. Once the heart ceases to function, a healthy human brain can survive without oxygen for up to 4 minutes without suffering permanent damage. But while typical Emergency Medical Service response time is only a few minutes, in remote or difficult to access areas EMS may take 15 minutes or more to arrive.

HOW CPR WORKS
The air we inhale travels to the lungs where oxygen is picked up by our blood and then pumped by the heart to our tissue and organs. When a person experiences sudden cardiac arrest (SCA) - whether due to heart failure in adults and the elderly, or an injury such as near drowning, electrocution or severe trauma in a child - the heart goes from a normal beat to an arrhythmic pattern called ventricular fibrillation, and eventually ceases to beat altogether. This prevents oxygen from circulating throughout the body and reaching vital organs, rapidly killing cells and tissue. In essence, Cardio (heart) Pulmonary (lung) Resuscitation (revive, revitalize) serves as an artificial heartbeat and an artificial respirator.
WHEN TO ACTIVATE EMERGENCY MEDICAL SERVICES
It's critical to remember that dialing 9-1-1 (or your local emergency response number) may be the most important step you can take to save a life. If someone besides you is present, one of you should activate EMS immediately. However, if you're alone with the victim, call for assistance (EMS) should be made prior to starting CPR on an adult, but after 2 minutes of administering CPR on a child or infant.
ASSESSING THE SCENE
Always remember to exercise solid common sense. When faced with an emergency situation we may sometimes act impulsively and place ourselves in harm's way. Although time should not be wasted, remember to only approach the victim after determining that the scene is safe: always check for cars, fire, gas, downed electrical lines, and any other potential hazards before attempting to perform CPR.
CHAIN OF SURVIVAL
Beginning in 1991-92, the American Heart Association's CPR and Emergency Cardiac Care (ECC) guidelines adapted the concept of Chain of Survival, a series of actions that improve survival rates in victims of cardiac arrest.
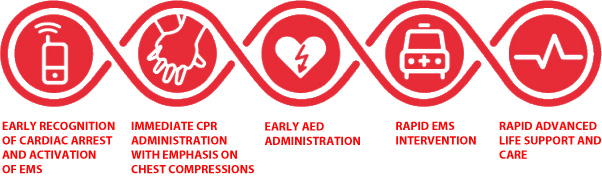
- The 5 "links" in this chain are:
- Prompt recognition of cardiac arrest and activation of EMS
- Immediate administration of CPR with emphasis on chest compressions
- Early defibrillation (AED)
- Rapid EMS intervention
- Rapid Advanced Life Support and care
LIABILITY
In most jurisdictions, the principle of Good Samaritan laws prevent negligence suits from being filed against any layperson (i.e. not medical professional) who makes a "good faith" effort to administer CPR or other forms of reasonable first aid assistance in an imminent emergency. However, it is worth noting that laws vary greatly from state to state and country to country.
DEFINITION
Because there is no single anatomic or physiologic characteristic that distinguishes an "adult" victim from a "child" victim and no scientific evidence that identifies a precise age to initiate Adult rather than Child CPR techniques, the ECC scientists made a consensus decision for age delineation that is based largely on practical criteria and ease of teaching. However, American Heart Association's guidelines dictate that adult CPR is performed on any person over the age of approximately 10 to 14 years, or post-adolescence, as defined by the presence of secondary sex characteristics (i.e. puberty).
ASSESSING THE SITUATION
Before attempting to provide assistance it's critical to first ensure that it's safe to approach the victim. For example, at a scene of an accident potential hazards can consist of traffic, fire, electric wires, etc. If you suspect that the victim has sustained spinal or neck injury, do not move or shake him.
- 1 PERSON CPR
- Verify that the victim is unresponsive by shaking the victim gently and shouting "Are you okay?"
- If there is no response, immediately activate EMS by dialing 9-1-1 (or local emergency response number)
- If AED is available, retrieve it
- Return to the victim and begin CPR (and use the AED as appropriate)
- 2 PERSON CPR
- Verify that the victim is unresponsive by shaking the victim gently and shouting "Are you okay?"
- One of the rescuers should immediately activate EMS by dialing 9-1-1 (or local emergency response number) and if AED is available, retrieve it
- Simultaneously, the second rescuer should remain with the victim to begin CPR
- Both rescuers should continue to perform CPR (and use AED as appropriate)
PERFORMING CPR
Studies of out-of-hospital adult cardiac arrest incidents have shown that survival rate was significantly higher whenever bystanders attempted to administer CPR with emphasis on blood flow and not solely on the precise sequence of compressions and rescue breaths. In other words, rather than not attempt CPR for fear of doing it incorrectly, it is more important to remember to push vigorously (i.e. hard and fast) than to remember exactly how many times to push.
Before commencing CPR first determine if the victim has a pulse. To do this in an adult victim, place two fingertips on his carotid artery which is located in the depression between the windpipe and the neck muscles, and apply slight pressure for several, but no more than 10, seconds. At the same time observe the victim's chest and face for signs of normal breathing. If no pulse is detected or you are not sure, it's best not to waste precious moments, and to immediately begin chest compressions.
"C" is for COMPRESSIONS
Place two fingers of one hand on the victim's sternum [show me] and then place the heel of your other hand just above your fingers [show me]. Now place your hand on top of that hand [show me] and interlace the fingers [show me]. Lock your elbows and using your body's weight, compress the victim's chest to the depth of at least 2 inches for an average adult, not exceeding 2.4 inches - a good way to remember is 2 hands, 2 inches [show me] - at a brisk rate of 100 to 120 compressions per minute (that's nearly 2 compressions per second). If possible, avoid leaning on the victim's chest between compressions in order to allow full recoil after each compression.
"A" is for AIRWAY
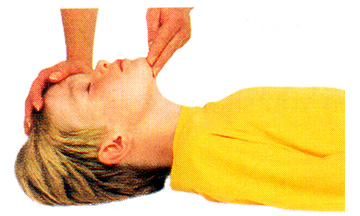
If the victim is unconscious and is unresponsive, you need to make sure that his airway is clear of obstructions. The tongue is the most common airway obstruction in an unconscious person and it may be necessary to perform a finger sweep to move the tongue or any other foreign object away from the air passage. With the victim lying flat on his back, firmly hold his chin with one hand while using the finger of your other hand in a sweeping motion [show me] as you sweep it out of the airway. Once the airway is unblocked, place your hand on victim's forehead and your other hand under the tip of the chin and gently tilt his head backward [show me]. In this position (head tilt/chin lift) the weight of the tongue will force it to shift away from the back of the throat, unblocking the airway. If the victim is still not breathing on his own after the airway has been cleared, you will have to assist him breathing.
"B" is for BREATHING (you may skip this section if you are performing compression-only CPR)
While supporting the victim's chin so as to keep it lifted up and the head tilted back, pinch his nose to prevent air from escaping once you begin to ventilate [show me]. Take a full breath, place your mouth tightly over the victim's (use a shield barrier if one is available) and blow [show me] for approximately 1 second as the victim's chest rises. Do this twice (2 breaths) while maintaining a tight seal around his mouth. Be careful not to over-inflate his lungs as this may force air into the stomach, causing the victim to vomit. If this happens, turn the victim's head to the side and sweep any obstructions out of the mouth before proceeding. Between each breath allow the victim's lungs to relax - place your ear near his mouth and listen as the air escapes and watch the chest fall as he exhales [show me]. If the victim remains unresponsive (no breathing, coughing or moving), check his circulation.
1 PERSON CPR CYCLE
Repeat the above sequence by counting aloud as you compress 30 times at the rate of 100-120/minute, while minimizing pauses between compressions. Allow full recoil of chest after each compression; do not lean on the chest after each compression. Finish the cycle by giving the victim 2 breaths. This cycle should be performed 5 times - 30 compressions followed by 2 breaths - after which the victim's carotid artery should be checked for pulse and he should be observed for other signs of consciousness. If you do not feel a pulse within 10 seconds, you should begin chest compressions and ventilations again and continue until AED is available, EMS arrives, or the victim regains consciousness.
2 PERSON CPR CYCLE
Repeat the above sequence by counting aloud as you compress 30 times at the rate of 100-120/minute, while minimizing pauses between compressions. Allow full recoil of chest after each compression; do not lean on the chest after each compression. Finish the cycle by giving the victim 2 breaths. To prevent fatigue and deterioration in quality and rate of chest compressions the rescuers should change compressor and ventilator roles every 2 minutes but the switch should be accomplished as quickly as possible to minimize interruptions in compressions. The victim's carotid artery should be checked for pulse and he should be observed for other signs of consciousness. If you no pulse is detected within 10 seconds, you should begin chest compressions and ventilations again and continue until AED is available, EMS arrives, or the victim regains consciousness.
DEFINITION
In accordance with current American Heart Association's guidelines, healthcare providers and laypersons should administer Child CPR to any victims ranging from about 1- to approximately 10 to 14 years of age, or the onset of adolescence as defined by the presence of secondary sex characteristics (i.e. puberty).
ASSESSING THE SITUATION
Before attempting to provide assistance it's critical to first ensure that it's safe to approach the victim. For example, at a scene of an accident potential hazards can consist of traffic, fire, electric wires, etc. If you suspect that the victim has sustained spinal or neck injury, do not move or shake him.
One of the most important distinctions between adult and child CPR is that in children primary respiratory arrest is more commonly caused by an injury such as poisoning, smoke inhalation, drowning, head trauma, etc. rather than sudden cardiac arrest (SCA). As such, statistics have shown that a child victim is more likely to respond to, and to benefit from, the immediate administration of CPR.
- 1 PERSON CPR
- Verify that the victim is unresponsive by gently shaking him and, if age-appropriate, shouting "Are you okay?"
- Begin CPR by providing 5 cycles of 30 compressions and 2 ventilations, for approximately 2 minutes
- Activate EMS by dialing 9-1-1 (or local emergency response number)
- If AED is available, retrieve it
- Return to the victim and begin CPR (and use the AED as appropriate)
- 2 PERSON CPR
- Verify that the victim is unresponsive by gently shaking him and, if age-appropriate, shouting "Are you okay?"
- One of the rescuers should immediately begin CPR
- Simultaneously, the second rescuer should activate EMS by dialing 9-1-1 (or local emergency response number) and if AED is available, retrieve it
- Both rescuers should continue to perform CPR (and use AED as appropriate)
PERFORMING CPR
Studies have shown that survival rate improved significantly whenever bystanders attempted to provide CPR, with emphasis on blood flow and not solely on the exact sequences of compressions and rescue breaths. In other words, rather than not attempt CPR due to fear of doing it incorrectly, it is more important to remember to push vigorous (i.e. hard and fast) than to remember exactly how many times to push.
Before commencing CPR first determine if the victim has a pulse. As with an adult victim, a child's pulse is checked at the carotid artery by placing two fingertips and applying slight pressure for no more than 10 seconds. At the same time observe the victim's chest and face for signs of normal breathing. If no pulse is detected or you are not sure, it's best to immediately begin chest compressions.
"C" is for COMPRESSIONS
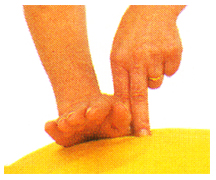
When performing chest compressions on a child proper hand placement is the same as with adults. Place two fingers at the sternum and then place the heel of your other hand directly above your fingers [show me]. Depending on a child victim's size, only one hand may be used for compressions of about about 2 inches or one-third (1/3) chest depth [show me], at a brisk rate of 100 to 120 compressions per minute (that's nearly 2 compressions per second). Avoid leaning on the victim's chest between compressions in order to allow full recoil after each compression. If you feel or hear slight cracking sound, you are pressing too hard. Do not become alarmed and do not stop your rescue efforts! Apply less pressure as you continue compressions.
"A" is for AIRWAY
A distressed child's breaths may be faint and shallow - closely look, listen and feel for any signs of breathing. If no breathing is detected, the tongue or a foreign object may be obstructing the airway. Exercise extra when you open the victim's air passage using the head tilt/chin lift technique [show me] which will shift his tongue away from the airway. Sweep away any foreign matter. If the child is still not breathing after the airway has been cleared, assist him in breathing.
"B" is for BREATHING (you may skip this section if you are performing compression-only CPR)
While supporting the child's chin keeping it lifted up and the head tilted back, pinch his nose - or for a smaller child, cover his mouth and nose with your mouth - to create a tight seal prevent air from escaping once you begin to ventilate ((use a shield barrier if one is available). Give 2 breaths [show me] for approximately 1 second each. Keep in mind that depending on the age and size, a child's lungs may have much smaller capacity than those of an adult. When ventilating a child, be sure to use shallower breaths and keep an eye on the his chest to avoid stomach distention. If this happens and the child vomits, turn his head sideways and sweep all obstructions out of the mouth before proceeding. Between each breath allow the victim's lungs to relax - place your ear near his mouth and listen as the air escapes and watch the chest fall as he exhales. If the child victim remains unresponsive (no breathing, coughing or moving), check his circulation.
1 PERSON CPR CYCLE
Repeat the above sequence counting aloud as you compress 30 times at the rate of 100-120/minute, while minimizing pauses between compressions. Allow full recoil of chest after each compression; do not lean on the chest after each compression. Finish the cycle by giving the victim 2 breaths. This cycle should be performed 5 times - 30 compressions followed by 2 breaths - after which the child victim's carotid artery should be checked for pulse and he should be observed for other signs of consciousness. If you do not feel a pulse within 10 seconds, you should begin chest compressions again and continue until AED is available, EMS arrives, or the victim regains consciousness.
2 PERSON CPR CYCLE
Repeat the above sequence by counting aloud as you compress 30 times at the rate of 100-120/minute, while minimizing pauses between compressions. Allow full recoil of chest after each compression; do not lean on the chest after each compression. Finish the cycle by giving the victim 2 breaths. To prevent fatigue and deterioration in quality and rate of chest compressions the rescuers should change compressor and ventilator roles every 2 minutes but the switch should be accomplished as quickly as possible to minimize interruptions in compressions. The victim's carotid artery should be checked for pulse and he should be observed for other signs of consciousness. If you no pulse is detected within 10 seconds, you should begin chest compressions and ventilations again and continue until AED is available, EMS arrives, or the victim regains consciousness.
DEFINITION
Infant CPR is administered to any victim under the age of 12 months except for neonatal victims (i.e. newborns in the first hours after birth). Infants, just as children, have a much higher chance of survival if CPR is administered immediately.
ASSESSING THE SITUATION
Before attempting to provide assistance it's critical to ensure that it's safe to approach the victim. For example, at a scene of an accident potential hazards can consist of traffic, fire, electric wires, etc. If you suspect that the victim has sustained spinal or neck injury, do not move or shake him.
As with child victims, primary respiratory arrest in infants is more commonly caused by an injury (for example, poisoning, smoke inhalation, drowning, head trauma, etc.), rather than sudden cardiac arrest (SCA). As such, statistics have shown that an infant victim is more likely to respond to, and to benefit from, the immediate administration of CPR. Currently there is no single consensus on recommendation for or against the use of AED's for infants.
- 1 PERSON CPR
- Verify that the infant victim is unresponsive by patting his feet and gently tapping his chest or shoulders
- Begin CPR by providing 5 cycles of 30 compressions and 2 ventilations, for approximately 2 minutes
- Activate EMS by dialing 9-1-1 (or local emergency response number)
- If AED is available and you choose to use it, retrieve it
- Return to the victim and begin CPR (and use the AED as appropriate)
- 2 PERSON CPR
- Verify that the victim is unresponsive by patting his feet and gently tapping his chest or shoulders
- One of the rescuers should immediately begin CPR
- Simultaneously, the second rescuer should activate EMS by dialing 9-1-1 (or local emergency response number) and if AED is available, retrieve it
- Both rescuers should continue to perform CPR (and use AED as appropriate)
PERFORMING CPR
Studies of out-of-hospital adult cardiac arrest incidents have shown that survival rate was significantly higher whenever bystanders attempted to administer CPR with emphasis on blood flow and not solely on the precise sequence of compressions and rescue breaths. In other words, rather than not attempt CPR for fear of doing it incorrectly, it is more important to circulate oxygenated blood by pushing fast than to remember how many times to push.
Before commencing CPR you must first check the victim for pulse. Unlike with an adult or child, an infant's pulse is checked at the brachial artery which is located inside of the upper arm, between the elbow and the shoulder. Locate the artery and place two fingers on it, applying slight pressure for 5 to 10 seconds. If unsure or you definitely do not feel a pulse within that timeframe, it's best to immediately begin chest compressions.
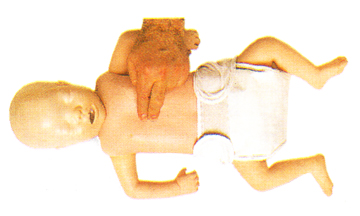
"C" is for COMPRESSIONS
An infant's delicate ribcage is especially susceptible to damage if chest compressions are improperly performed, therefore it is important to use caution when rescuing an infant. With the infant victim flat on his back, place two fingers in the center of his chest at or just below the nipple line [show me]. The compression should be approximately one-third (1/3) to one-half (1/2) the depth of the chest. A good way to remember this is half-hand, half-chest deep.
"A" is for AIRWAY
An infant may to take extremely shallow and rapid breaths, so carefully look, listen and feel for normal breathing. If you cannot detect any signs of breathing, the tongue or a foreign object may be obstructing the airway. Although the head tilt/chin lift technique is similar to adults and children, when clearing an infant's airway it's important not to tilt the head too far back as an infant's airway is extremely narrow and overextending the neck may actually close off the air passage [show me]. Tilt the head back into what is sometimes known as the "sniffer's position" - far enough to make the infant look as if he is sniffing - which will shift his tongue away from the airway, and if necessary, sweep away any foreign matter. If the child is still not breathing after the airway has been cleared, assist him in breathing.
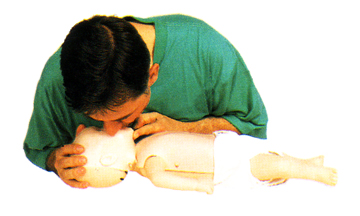
"B" is for BREATHING (you may skip this section if you are performing compression-only CPR)
To artificially respirate an infant, place your mouth over his mouth and nose creating a tight seal and give 2 gentle puffs from your cheeks [show me]. Let the victim exhale between breaths - again, watch his chest closely and listen and feel for faint breathing. If the infant victim remains unresponsive (no crying or moving), immediately check his circulation.
1 PERSON CPR CYCLE
Repeat the above sequence counting aloud as you compress 30 times at the rate of 100-120/minute, while minimizing pauses between compressions. Allow full recoil of chest after each compression. Finish the cycle by giving the victim 2 breaths. This cycle should be performed 5 times - 30 compressions followed by 2 breaths - after which the infant's brachial artery should be checked for pulse and he should be observed for other signs of consciousness. If you do not feel a pulse within 10 seconds, you should begin chest compressions again and continue until AED is available, EMS arrives, or the victim regains consciousness.
2 PERSON CPR CYCLE
Repeat the above sequence by counting aloud as you compress 30 times at the rate of 100-120/minute, while minimizing pauses between compressions. Allow full recoil of chest after each compression; do not lean on the chest after each compression. Finish the cycle by giving the victim 2 breaths. To prevent fatigue and deterioration in quality and rate of chest compressions the rescuers should change compressor and ventilator roles every 2 minutes but the switch should be accomplished as quickly as possible to minimize interruptions in compressions. The victim's carotid artery should be checked for pulse and he should be observed for other signs of consciousness. If you no pulse is detected within 10 seconds, you should begin chest compressions and ventilations again and continue until AED is available, EMS arrives, or the victim regains consciousness.